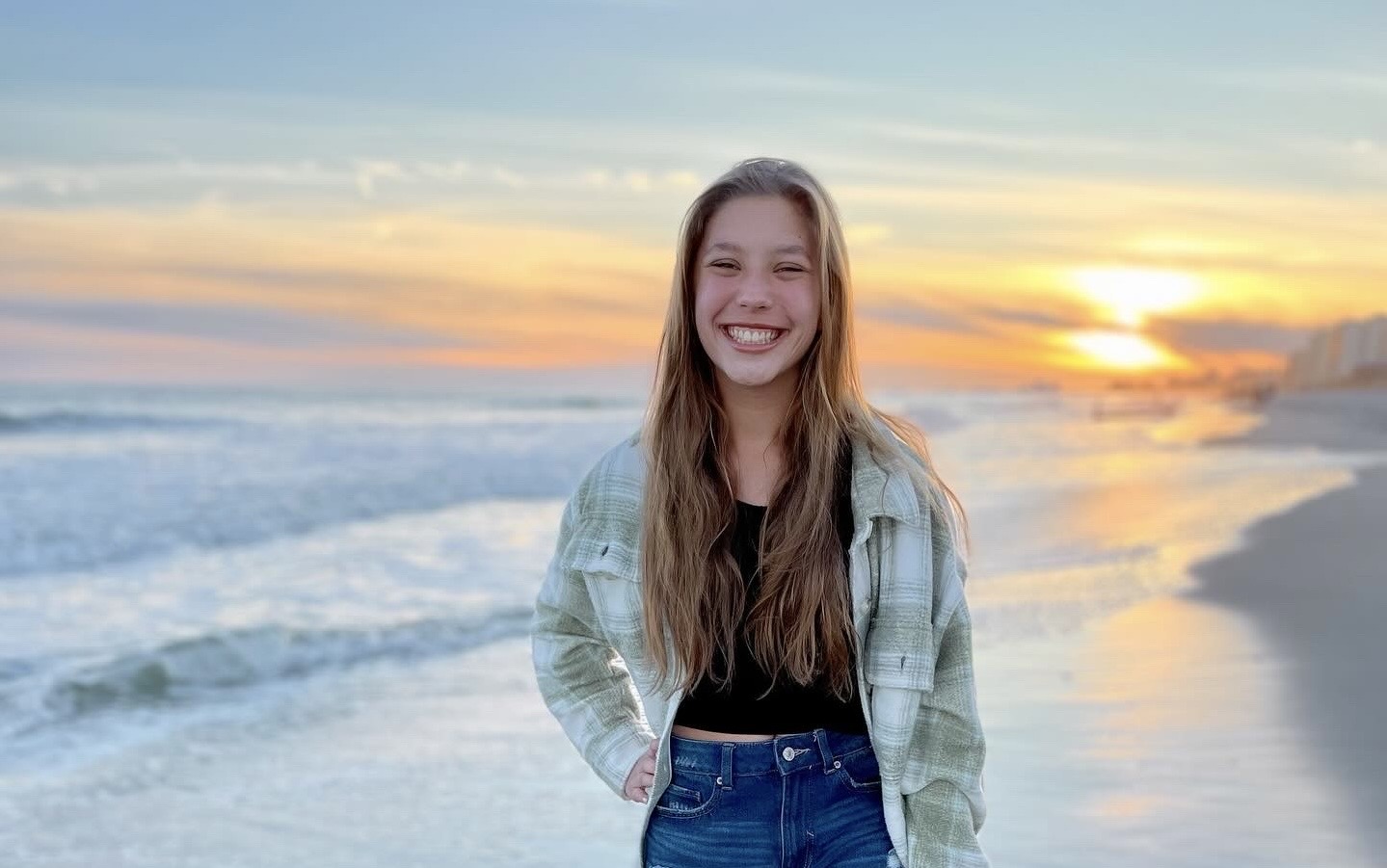
Heart Warrior Elena Thrives Years after D-TGA Diagnosis
When Elena had life-saving heart surgery at just two days old, her mom Amanda says they must have poured a little extra love and kindness in before they closed her up. Going from a devastating diagnosis of Dextro-Transposition of the…
High Blood Pressure in Children: Not Just an Adult Problem
Blood pressure is the measurement of the force inside a person’s blood vessels as blood pushes through. High blood pressure means that the force is higher than normal levels for a person’s gender, size and weight and can lead to…
Physicians with Heart: Dr. William McEachern
Children’s Healthcare of Atlanta Cardiology pediatric cardiologist William McEachern, M.D., knew when he was in medical school that he was best suited to work as part of a fast-moving team that managed the most complex cases of congenital heart disease.…
I Wish I Would’ve Known How Strong She Is
Sending a child to kindergarten with a CHD diagnosis can be nerve-wracking. But when Katie looks back on that day now, she can only be amazed by all her daughter has accomplished. Born 21 years ago at just four pounds…
Nurse Practitioners with Heart: Heather Jordan
When Heather Jordan, pediatric cardiology nurse practitioner, graduated from the University of Louisville and an accelerated nursing program, she wanted to apply to Children’s Healthcare of Atlanta. Coming from out of state, she wasn’t sure how to begin the process,…
Heart Warrior Rudy Loves Church, Hugs and WWE Wrestling
Eight-year-old Rudy’s mom, Heidi, said her family’s world was flipped upside down when her son had three open heart surgeries in two years to correct his CHDs. But she looks at him today and sees strong little boy who loves…
Physicians with Heart: Dr. Chad Mao
After 15 years of military service as a United States Navy medical officer, Chad Mao, MD, says the singular focus on the care of children by Children’s Healthcare of Atlanta Cardiology makes his work fun. Dr. Mao is the medical…
Heart Warrior Mom Now Educates Others About Children’s Cardiology
After a typical pregnancy and uneventful delivery, Holly and Dan didn’t expect to be doing anything other than enjoying the birth of their second daughter with their family. But just hours after Annabelle’s birth, they discovered she had a rare…
The Littlest Heart Warriors Can Move Mountains
Even before Everleigh Faith came into the world, her name marked her as a miracle child who would overcome great obstacles. Diagnosed with Tetralogy of Fallot, Pulmonary Atresia and MAPCAS (Major Aortopulmonary Collateral Arteries), her congenital heart disease (CHD) journey…
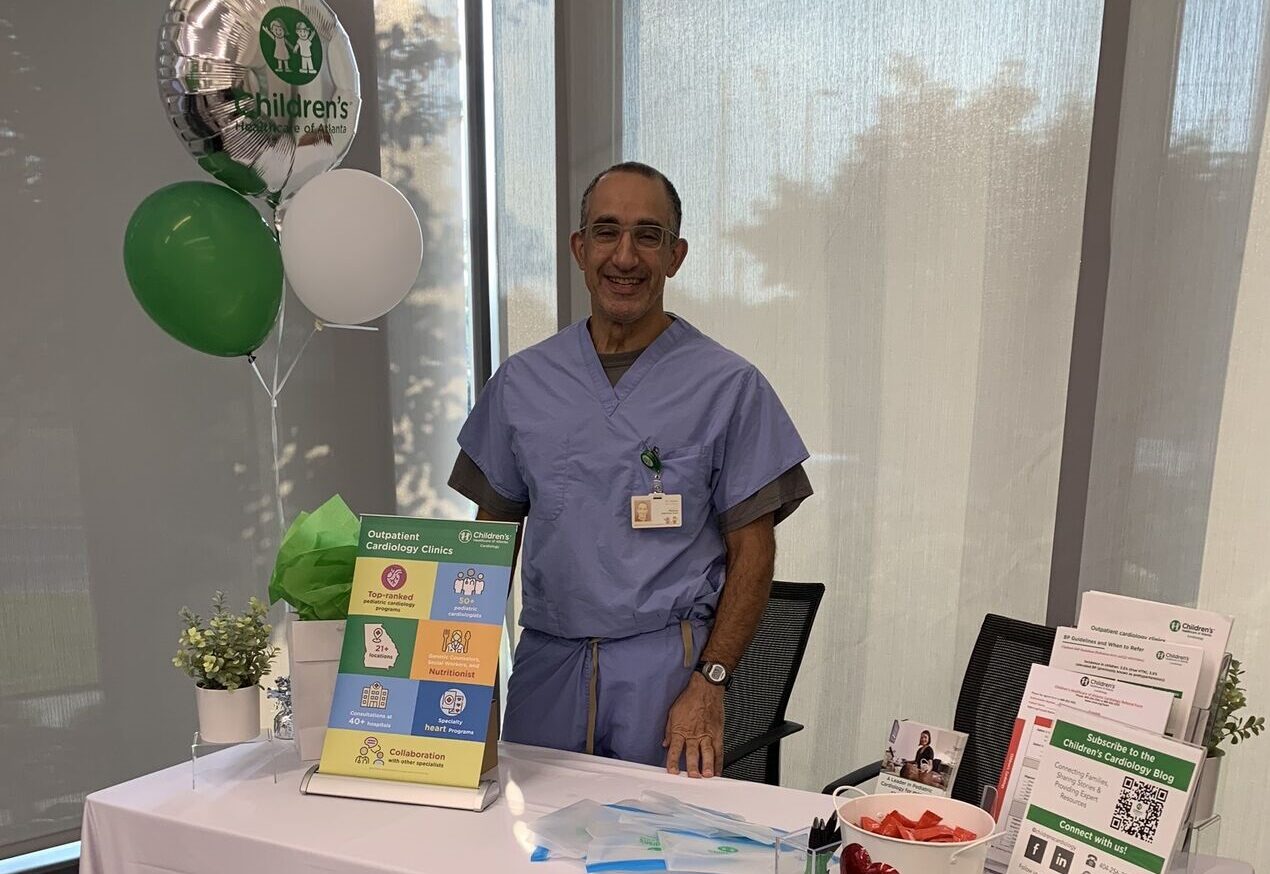
Physicians with Heart: Dr. Cyrus Samai
According to pediatric cardiologist Cyrus Samai, MD, one of the most important things Children’s Healthcare of Atlanta Cardiology brings to Georgia families is its focus on improving access to top quality cardiac care across the state. By hiring pediatric cardiologists…