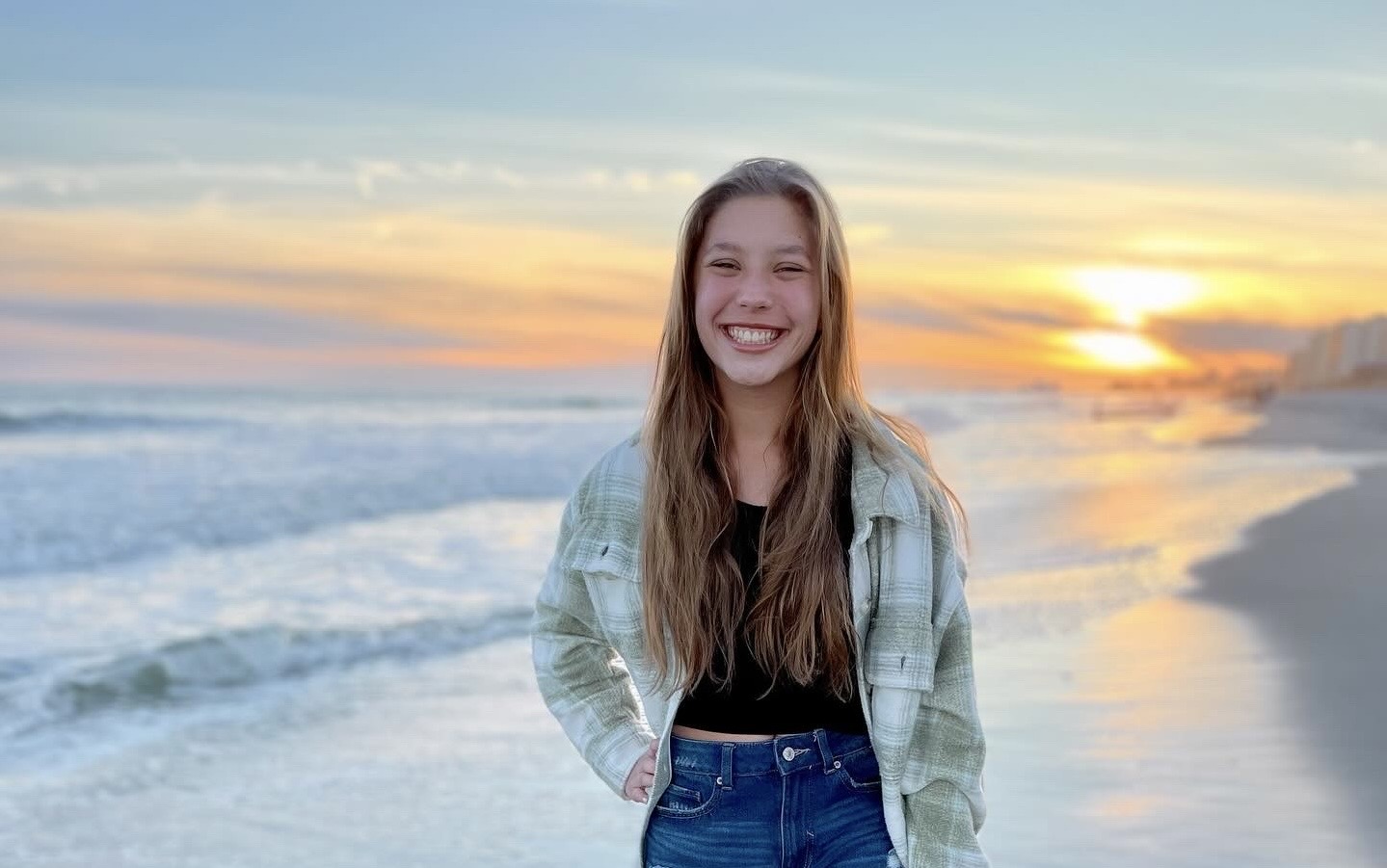
Heart Warrior Elena Thrives Years after D-TGA Diagnosis
When Elena had life-saving heart surgery at just two days old, her mom Amanda says they must have poured a little extra love and kindness in before they closed her up. Going from a devastating diagnosis of Dextro-Transposition of the…